Sarah Killcoyne, Postdoctoral Fellow at EMBL’s European Bioinformatics Institute, discusses a newly-developed statistical model that uses genomic sequencing to accurately predict the risk of a patient with Barrett’s oesophagus developing cancer.
Oesophageal cancer is the eighth most common cancer worldwide. The most common subtype in the UK, Europe, and the USA (oesophageal adenocarcinoma) develops from a condition called Barrett’s oesophagus. Existing monitoring and treatment methods are very intrusive, and many patients have to undergo burdensome procedures to ensure that no cancer is missed.
Now, researchers at the University of Cambridge (UK), the European Molecular Biology Laboratory’s European Bioinformatics Institute (EMBL-EBI), and collaborators have developed a statistical model that uses genomic data to accurately predict whether a patient with Barrett’s oesophagus has a high or low risk of developing cancer.
Sarah Killcoyne, Visiting Postdoctoral Fellow at EMBL-EBI and co-author of the new research, which has been published in Nature, spoke to The Innovation Platform about how the new method can both help to earlier identify those patients with Barrett’s at high risk of developing oesophageal cancer, as well as those at lower risk, thereby reducing the need for invasive surveillance procedures.
Perhaps you could begin by explaining how oesophageal cancer is typically diagnosed, as well as the surveillance procedures that patients normally have to undergo?
The research in the newly-published paper focuses on Barrett’s oesophagus, which is a pre-cancerous condition to oesophageal adenocarcinoma. Barrett’s oesophagus is not dangerous in itself, but it does mean that a patient is at a higher risk of developing cancer.
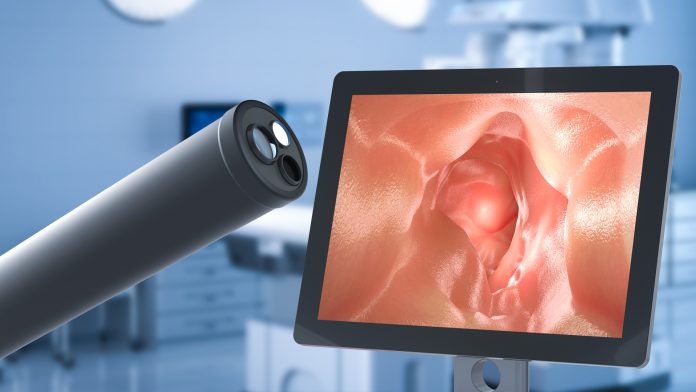
Barrett’s is diagnosed by administering an endoscopy and taking oesophageal biopsies, usually to patients who have presented with symptoms of sustained gastroesophageal reflux disease (GERD). If Barrett’s is confirmed, then patients have to undergo monitoring with a repeat endoscopy, usually every two to three years.
The endoscope is an illuminated tube with a camera at the end which is passed through the mouth and down the oesophagus as far as the stomach. While this is considered a minimally invasive procedure, it can be very uncomfortable, with some patients not tolerating it very well.
During the endoscopy examination, an expert gastrointestinal doctor will evaluate what the camera sees. Specifically, they are looking for changes in the Barrett’s that might suggest it is progressing towards cancer. These changes can be subtle and difficult to see. They will also take multiple biopsies, anything from four to 20 depending on how long the Barrett’s is, which will be sent to an expert gastroenterology pathologist to look for signs of dysplasia – whether the tissue is becoming more disordered and so more cancer-like (although not yet cancerous).
Should a patient be diagnosed with high-grade dysplasia, or early cancer, a treatment that can be performed through the endoscope – known as mucosal resection or radiofrequency ablation – will be recommended. These techniques involve performing micro-surgery through the endoscope or using radiofrequency energy to burn out the first layer of tissue, thereby removing the cells that are becoming cancerous. This is a relatively simple treatment that can prevent cancer from occurring.
Currently, the only real method we have of identifying whether a patient with Barrett’s is at risk of developing cancer is by the grading of biopsies that is provided by the pathologists. While high-grade dysplasia means there is a very high risk of the patient developing oesophageal adenocarcinoma, and it is straightforward to identify and remove it, there are grades below that, such as low grade or indefinite dysplasia, and often pathologists don’t necessarily agree on what it is that they are seeing and it is less straightforward to assess how much risk it presents. Because of this, particularly in the UK and the USA, patients with low-grade dysplasia are often treated as though they have high-risk dysplasia, which may mean that they are undergoing treatments that they don’t actually need.

You have now developed a statistical model that uses genomic data to accurately predict whether a patient with Barrett’s oesophagus has a high or low risk of developing cancer. How was this achieved? What were the biggest challenges?
Our model utilises some fairly new genomics technologies. We have been using high depth whole genome sequencing in tumours for some time now to try to better understand the mutations that are occurring. But this is an extremely expensive technology.
For our new research, we have employed what is known as a ‘low resolution or ‘shallow sequencing’, which is relatively inexpensive – around £100-£200 compared to £1,000-£2,000 per sample of high depth sequencing. However, shallow sequencing also provides significantly less resolution on the data itself. Perhaps the biggest challenge was thus to develop a process for generating data that was clean enough to be usefully interpreted, because any kind of really low-resolution data is incredibly noisy, which is a significant concern when attempting to develop statistical models.
Developing patient cohorts was also a challenge. Most patients with Barrett’s will never develop cancer but will undergo surveillance for a number of years. Identifying a cohort of patients that included some who eventually transitioned to cancer was a huge amount of work. This was performed by my co-author, Eleanor Gregson, and it took her a couple of years to put the cohort together and to gather the historical tissues that had been saved.
Beyond that, there are always challenges when it comes to understanding and interpreting new data.
What were the most significant findings from the research, and what are the biggest benefits for patients?
The most significant finding is that we have been able to sensitively identify patients years before their clinical diagnosis: there were patients in our data set that had been under surveillance for 15 years, and we were able to reliably say that at least half of those patients for whom we had more than eight years of data before they had been diagnosed were at high risk of developing cancer. That reliability increased the closer in time we got to their diagnosis.
Almost as important was that these risks were fairly stable over time. That is, we can identify very early on those patients either at high or low risk, as the level of risk was consistent. This means there is a case for potentially changing the way patients receive treatment, which would be the biggest benefit for them – those at high risk could be offered treatment much earlier, so they are less likely to develop cancer, while those at lower risk could have the frequency of surveillance decreased so they are not undergoing invasive procedures such as endoscopies so often.
The research involved collaboration between computational biologists and clinician-scientists. Were there any challenges here?
I am a computational biologist while Gregson is an experimental biologist and initiated the project. She, therefore, did much of the interfacing with clinicians – though I would also work with them after the fact to try to understand the aetiology of the disease.
Of course, there is always a learning curve; certainly, from my side, in understanding what the clinical meaning of certain terms are, for instance, and whether or not a particular finding is in fact clinically meaningful. Just as there is in translating these risks into terminology that is useful for clinicians. Indeed, the way I might describe something to another computational biologist would be very different to how the same thing would need to be communicated to a clinician, and so we have always been mindful of that because one of the main goals for us has been to make the new model clinically useful and practical.
Next steps involve refining the method before advancing to clinical trials. What progress is being made here? Do you have an anticipated timeframe before the model can be rolled out?
It is perhaps too early to talk about timeframes in that sense. One of the next steps for us is to enrol more patients, both retrospectively and prospectively, and to ensure that the accuracy of the new model and the algorithms we are developing and employing do not compromise patient safety. Our recent study generated a lot of data, but it is still a relatively small number of patients.
We also want to bring in more data types; we want to bring in the clinical information that pathologists were already using, as well as information about the pathology itself. That way, we may be able to learn more from the dysplastic tissues. This study focused on the genomics, so we really wanted to make sure that it was independent of these other factors. But now, we need to bring these other factors back in.
Finally, there is hope that the model may be extended to other cancer types in the future. How do you envisage this happening? What will need to be achieved? Will clinical trials need to be completed first?
No, I don’t believe that there is a need to wait until the completion of clinical trials for Barrett’s oesophagus patients; the method and the algorithm can certainly start to be expanded now.
The question, however, is around the accessibility and availability of pre-cancerous tissues. One of the benefits of working with the oesophageal tissue is that although it is uncomfortable for patients, the oesophagus is a very accessible organ. But when you start looking at pre-cancerous tissues for other internal solid cancers, it gets more difficult. The information is there in some cases, and so perhaps this model might be more easily extended to areas such as breast or colon cancer, where we have some idea of pre-cancerous tissues and regular clinical surveillance is already performed.
Sarah Killcoyne
Postdoctoral Fellow
The European Bioinformatics Institute (EMBL-EBI)
sk875@mrc-cu.cam.ac.uk
Tweet @emblebi
www.ebi.ac.uk/
Please note, this article will also appear in the fourth edition of our new quarterly publication.