Christian Lodberg Hvas and Simon Mark Dahl Jørgensen, from the Department of Hepatology and Gastroenterology at Aarhus University Hospital, Denmark, discuss C. diff infection and faecal transfer.
Recently renamed from Clostridium difficile and known as C. diff, Clostridioides difficile – is a spore-forming micro-organism that causes severe colitis in more than 300,000 Europeans every year. Up to one third suffer a relapse of the disease after antibiotic therapy. Transfer of health donor faeces – a faecal microbiota transplantation, or FMT – provides sustained cure from the disease in nine out of 10 patients treated for recurrent C. diff infection. The establishment of FMT services is underway in several countries, but this puts high demands on infrastructure, ensuring patient safety and regulation from health authorities.
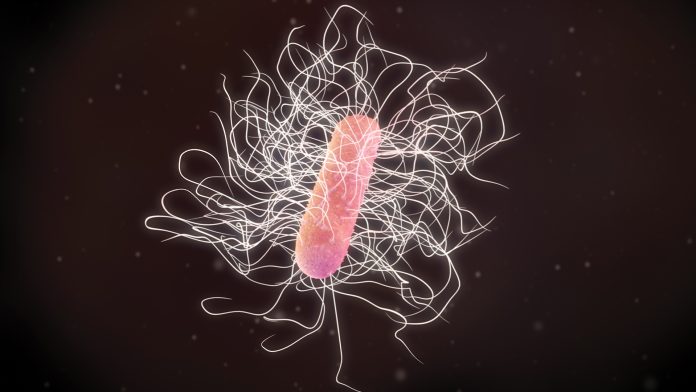
C diff: a killer bug
When exposed to a hostile environment, C. diff survives as endospores that are highly resistant and ubiquitously present in etc soil, water and the intestines. A part of the commensal bacterial ecosystem of the human gut, it is usually kept under strict control from hundreds of different strains. Together, these constitute the human intestinal microbiota, or the gut flora. Under normal circumstances, the intestinal microbiota ensures a stable gut function and general health of the host, helping to digest nutrients, produce short chain fatty acids, vitamins, etc.
This delicate balance may be disturbed by antibiotic treatment, therapies such as proton pump inhibitors used for acid-related disease, or a weakened immune system. If C. diff overgrowth eventually occurs in the large intestine, overt disease may develop, manifesting as diarrhea, abdominal pain and distension, fever, and ultimately organ failure and death. If left untreated, mortality from C. diff infection is high, and even with targeted antibiotic therapy, mortality approaches 20%. The elderly and hospitalised patients are particularly prone to developing severe disease, and severe C. diff infection poses a serious public health challenge to Western societies. Still, severe disease may develop in young, healthy individuals without prior disease or treatment.
The epidemic of C. diff stands in the shadow of the widespread use of broad spectrum antibiotics that has evolved in the western world during the past half century. In addition, profound lifestyle changes have changed the intestinal microbiota on a population level. C. diff infection represents the ultimate breakdown of the intestinal ecosystem. One may speculate if the epidemic of this primitive imposter evolved alongside the development of an impoverished intestinal ecosystem in modern man.
The gut ecosystem
Since the millennium, we have gained insight into the complex interplay between our intestinal microbiota and the development of metabolic and immune diseases. Our understanding of the individual composition of our intestinal microbiota has evolved through ambitious national and international research conglomerates such as the Human Microbiome Project and MetaHIT. Modern gene sequencing techniques have allowed a detailed mapping of the inner life of large cohorts of healthy volunteers and, later, patients suffering from specific diseases. Its cause and effect remain unresolved.
Bacterial composition and diversity has long been the focus of research and treatment development. Only recently has attention been drawn to an even more complex ecosystem that unfolds inside the bacteria, in the form of bacteriophages, or viruses. The virome has gained increased attention and may play a key part in educating the human immune system and conferring treatment effects during faecal transfer.
Our understanding of how microbiota-based treatments may manipulate the gut ecosystem is still in its infancy. Both the bacterial microbiota and the virome may be key players.
Prevention and treatment of C. diff infection
Prevention of the development of C. diff infection is key. This includes antibiotic stewardship and the rigorous maintenance of hospital hygiene standards. Several quality improvement initiatives have been documented as effective to limit the spread of C. diff infection among hospitalised patients.
Once clinical disease has developed in a patient, conventional treatments include antibiotics such as metronidazole, vancomycin, and the recently marketed drug fidaxomicin. Prices vary greatly, from €1 per day for metronidazole to over €27 for vancomycin to €127 per day for fidaxomicin (prices in Denmark, May 2019). A monoclonal antibody that targets the B toxin of the bacteria may lower the relapse rate when given during antibiotic therapy, bezlotoxumab (Zinplava®). The drug is marketed at €3,600 per treatment. Treatment algorithms are currently being debated in scientific societies.
Although antibiotics are superior to placebo and the addition of antibody treatment may further lower relapse rate, disease recurrence is frequent – up to 40%. In patients with multiple recurrences, the recurrence rate following treatments such as vancomycin approaches 80%. New treatments are therefore warranted.
Faecal transfer – a life-saving therapy for C. diff infection
The transfer of faeces from a healthy donor is known as ‘faecal microbiota transplantation’ (FMT). First described in written sources from Ancient China and renaissance Italy, it was first reported in modern science in 1958. A surgeon in Denver, Colorado, USA, Ben Eiseman, reported the dramatic cure of four critically ill patients who suffered from pseudomembranous colitis, which was then of unknown cause: the bacteria Clostridium difficile was described 20 years later, in 1978. His report, published in Surgery, formed the starting point of using FMT to treat patients with CDI. This was established as a final soluton in very few centers.
It caught almost no attention during the following 55 years where it was occasionally practiced in countries such as the USA and Finland. Then, in 2013, after having been hidden away in a drawer – so the story goes – a Dutch research group published the landmark trial with just 16 patients in the FMT arm, of whom 15 (94%) obtained resolution of recurrent C. diff, as compared with 27% of patients who had received high-dose vancomycin.
How does faecal transfer work?
The replacement of a disrupted microbiota with engraftment of the healthy donor microbiota in the recipient seems the obvious mechanism of action. Although this may hold some truth, it far from explains the dramatic effect observed in patients treated with FMT. Compared with other microbiota-based therapies such as purified bacterial mixes, or multidonor-based solution, conventional FMT is far superior in terms of clinical effect, with a universally reported effect rate of 85-95%. The whole package provides optimal effect.
Although engraftment occurs in most patients treated with FMT, clinical effect does not require engraftment of the donor microbiota.
Also, researchers who used sterile-filtrated faecal water obtained similar effect, indicating that bacteria-independent components of the donor microbiota contribute to the effect. These could be either viruses, metabolites from the microbiota, or host factors. Metabolites could include short-chain fatty acids, known to exert beneficial effects during everyday life: butyrate, valerate, etc. As intriguing as it may sound to isolate specific components and manufacture these as targeted super drugs, cryoconserved intact donor faeces seems the optimal cocktail to treat at least C. diff infection.
Promises for other diseases than C. diff?
Diseases where the occurrence has increased epidemically in the western-like parts of the world are in the searchlight when treatments to restore the impoverished gut ecosystem come to market. The association between the decline of classical infectious diseases such as rheumatoid fever, tuberculosis, and measles and the increase in autoimmune diseases such as allergies, multiple sclerosis, and inflammatory bowel diseases fed the hygiene theory, formulated in the 1990s.
Exposure to bacterial toxins through the respiratory system may prevent the development of asthma, as elegantly demonstrated by researchers who were allowed to sample dust from the houses and blood from the children of Amish communities in the Mid USA. The researchers coupled an unusually low occurrence of asthma with a fully developed immune response to domestic animal (horse) dust, which arose from the particular culture of the Amish that live closely together with many children and domestic animals – all factors known to harness a highly diverse intestinal bacterial microbiota, and apparently also a strong airway-mediated immune response that prevents asthma.
In relation to FMT, the relation between a disturbed intestinal microbiota and clinical disease has been established in diseases such as inflammatory bowel disease, diabetes mellitus, systemic lupus, and anchylosing spondylitis – that is, many of the diseases highlighted during the formulation of the hygiene theory. At the same time, public health threats such as obesity and irritable bowel syndrome are consistently correlated with alterations in the intestinal microbiota.
Given the dramatic effect of FMT in C. diff infection, it is speculated that similar effects could be obtained in these diseases. Although studies from animal models support this notion, clinical trials with FMT for these chronic conditions have provided conflicting evidence and no way near the magnitude of effects seen in C. diff.
Most importantly, there is a fundamental gap between C. diff as an ecosystem breakdown disease and chronic conditions with a fully established microbial community, as skewed as this may be. In time, specific subgroups of patients suffering from specific diseases may benefit from repeated FMT procedures. Until then, all treatments are carried out as part of clinical trials, with up to 60 scheduled treatments in some trials.
Setting up a FMT service
Both public hospitals and private clinics set out to establish clinics to offer FMT, focusing to variable degrees on profit or safety. Except from a few published consensus reports, no formal guidance or regulation from National health authorities exist as to how an FMT service is established. It may be useful to categorise an FMT service into three main domains:
- Donor recruitment and screening
- Laboratory processing
- Clinical application and follow-up.
Donor recruitment and screening may best be carried out by public centres which already hold the infrastructure and the expertise to guide and treat voluntary donors and handle large-scale donor screening and safety procedures. A question keeps drawing attention: is there such a thing as a super donor? Both donor and patient characteristics contribute to treatment efficacy, and in most diseases, some donors may prove better than others. Whether this is related to bacterial composition of the donor microbiota is unresolved.
Laboratory processing requires large-scale quality improvement and accreditation of quality standards and may also be best taken care of in institutions such as public blood centers.
Clinical application would be considered medical treatment in most European countries. It is usually performed by specialists in gastroenterology or infectious diseases, between institutions with access to advanced health care services such as microbiological diagnostics, endoscopy, outpatient and inpatient facilities, and multidisciplinary care. A follow-up of at least six months is common. Some patients experience complications such as bacterial overgrowth of the small intestine that requires specific treatment – a treatment that may increase the risk of C. diff recurrence. A balanced therapy approach is thus necessary.
Regulation from health authorities
Although the European Commission has formulated a legal framework appropriate for regulation of faecal transfer, the regulation of FMT from National health authorities differ in the European countries. The European Tissue and Cells Directive (EUTCD) specifies human cells and tissues, and only in a meeting report from 2014 are substances such as faeces and breast milk defined as substances of human origin (SoHo). Although not strictly human tissue, these are of similar character in a way that makes regulation according to the standards of the EUTCD sensible. In the case where microbiota-based products are refined into standardised biological agents, drug legislation may be the most appropriate regulative framework. It is currently unresolved exactly where the line between the two goes.
What the future holds
Faecal transfer has proven effective in specific diseases and may pave the way to eradicating recurrent C. diff infection. There are obvious limitations when trying to disseminate the treatment principle to other, chronic, disorders. Specific components of donor faeces may be developed into biological drugs aimed for certain conditions, and this poses particular challenges to legislation and safety.
Center for faecal microbiota transplantation (CEFTA) is supported by Innovation Fund Denmark (j.no. 8056-00006B)
Christian Lodberg Hvas and
Simon Mark Dahl Jørgensen
Department of Hepatology and Gastroenterology
Aarhus University Hospital
Department of Clinical Medicine
Aarhus University
+45 7845 3800
Christian.Hvas@auh.rm.dk
Tweet @AUHdk
www.cefta.com