By finding an effective way to treat patients at an early stage of cartilage damage we could delay or avoid the need for a total joint replacement.
Osteoarthritis (OA) is a degenerative joint disease typified by the degradation of cartilage and changes in the bone interface of a joint, resulting in pain, stiffness, and reduced mobility.1 According to the World Health Organisation, 52% of people over 70 years old have OA. This joint disease affects around 400 million people’s lives. This number will increase with an increasingly ageing population.2
Patients with osteoarthritis often suffer pain, loss of mobility, and go on to require a total joint replacement. These are major surgical procedures which are only undertaken when the disease has progressed to the stage where there is no alternative but a severely limited lifestyle. This can mean that patients will have suffered long periods of pain, discomfort, and reduced mobility before an operation is performed. In 2019, 240,550 joint replacements were performed in the UK (excluding Scotland) predominantly for osteoarthritis (see: www.njrcentre.org.uk/njrcentre/Healthcare-providers/Accessing-the-data/StatsOnline/NJR-StatsOnline). Developing a novel interventional strategy at an early stage of OA could potentially stop or delay the need for joint replacement and thus reduce the impact of the OA, both on personal and socio-economical levels.
Progression of osteoarthritis
In articulating joints, the articular cartilage, calcified cartilage, and subchondral bone form a composite unit referred to as the osteochondral unit. This has the unique capability of transferring loads during joint motion. Repetitive overloading to the joint could result in cartilage damage and changes in the subchondral bone, leading to mechanical instability of the joints and loss of joint function. Osteoarthritis is a chronic joint disease; it may start slowly with mild to moderate symptoms. During the progression of OA, thinning and degradation of articular cartilage, joint-space narrowing, osteophytes formation, and subchondral bone remodelling take place.3
Other pathological processes including microfractures, microedema, or microbleeding within the subchondral bone could lead to subchondral bone defects such as subchondral cyst formation.4 If the osteochondral defect has progressed to the stage where the patient’s quality of life has been significantly reduced and non-surgical treatments are no longer effective, then a joint replacement has to be performed in order to restore the function of the joint. However, this major surgical procedure often does not restore the full function of joints and has high long-term complication rates.
Osteoarthritis affects both cartilage and subchondral bone
Historically, OA had been looked at from a cartilage-centred perspective, but increasing evidence suggests that it should be considered as a ‘whole joint disease’5,6, even though some controversy still exists regarding the cascade of the pathological processes involved. The osteochondral unit has a thickness of around 3-5mm in adults; it consists of 90% articular cartilage, 5% of the calcified cartilage, and the remaining 5% the subchondral bone plate. Any alteration or disruption to this unit, the constituents, or their interface can result in ‘joint failure’ and development of clinical features of OA.
In subchondral bone, altered cellular function and increased remodelling lead to decreased bone density.7 As OA progresses, repetitive loading causes an imbalance between anabolic and catabolic chondrocyte activity. These changes are associated with the development of surface fibrillation, increased collagen breakdown, and fragmentation of the matrix, causing microcracks on the surface of the cartilage. Infiltration of blood vessels into cartilage and thickening of the cortical plate occurs in subchondral bone, with subsequent development of bone cysts, osteophytes, and deformations of subchondral bone contours.
Osteochondral scaffold innovation for early treatment of osteoarthritis
Treatments using tissue engineering methods have been established and are proving to be promising for the early treatment of OA. The goal of these methods is to repair the cartilage and osteochondral defects in the joint and restore its function. Earlier research has demonstrated that a cartilage-only approach resulted in poor cartilage fills, fibrocartilage formation, and the inappropriate integration of newly formed cartilage with the underlying subchondral bone. Subchondral bone and adjacent cartilage form a functional unit. An appropriate stable physical environment provided by the subchondral bone is crucial for the healthy growth of the overlying cartilage. To achieve better integration and cartilage fill, osteochondral scaffold therapy has been developed with a concept to regenerate the subchondral bone simultaneously with the regeneration of the overlying cartilage. Without support from the subchondral bone, the newly formed overlying cartilage would not get sufficient mechanical support and would collapse.
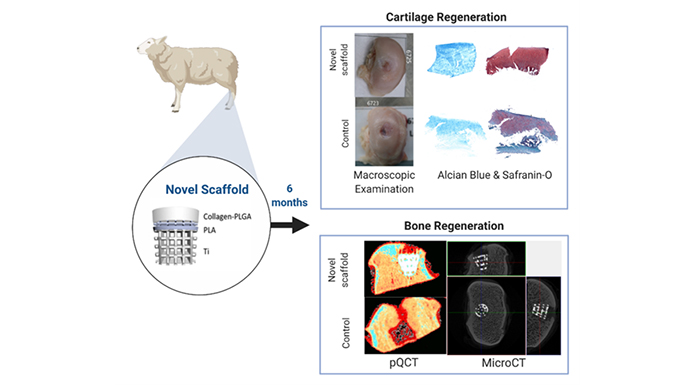
To this end, researchers at University College London (UCL) have invented a novel multi-layered osteochondral scaffold system which works with the body’s natural mechanisms to bear the load of the joint while encouraging the regeneration of cartilage and bone tissue. This novel scaffold incorporates both organic and inorganic material to make it customisable to each patient, a quality which, when scaled-up, would be an impressive advance for precision medicine, improving outcomes and the longevity of replacement joints and reducing the costs and risk factors of the knee and hip surgeries.
Both rabbit and sheep condyle model studies have demonstrated that the osteochondral scaffold achieved a stable mechanical fixation when implanted into the osteochondral defect of the joints – the bone grew into the titanium matrix and formed strong support to the overlying cartilage regeneration which led to the improved cartilage fill and healthy growth as revealed by histological examinations. The scaffold is designed for use with large bones like the knee, hip, and shoulder, but is flexible enough to be adapted to work with any joint in the body, large or small. Osteochondral scaffolds can be used to repair large cartilage defects in osteoarthritis patients to either delay the need for or act as a cost-effective alternative to joint replacement and will help patients to lead a more active and pain-free lifestyle.
This novel osteochondral scaffold technology is designed to repair and regenerate cartilage damage at an early enough stage to stop or slow down the progression of osteoarthritis. It is suitable for patients who have experienced trauma to a joint – perhaps caused by a sports injury, fall, or car accident. By finding an effective way to treat patients at an early stage of cartilage damage, we could delay or avoid the need for a total joint replacement.
We want to be able to offer early surgical intervention to patients which will relieve pain and help them to stay active, vastly improving their quality of life. Although total joint replacement is safe and effective, it is a major operation and is expensive to perform. Surgery using our scaffold technology will be faster and more cost-effective, which would benefit the NHS and should make a surgical solution accessible to more people with, or at risk of, osteoarthritis. This can reduce the financial burden to healthcare providers and the patients themselves. The beneficiaries reflect the value chain from the patient, through the clinician, the hospital and healthcare providers, to the industrial generators of the underpinning technology and materials. This will have a significant impact on clinical practice in the future.
References
- Martel-Pelletier, A.J. Barr, F.M. Cicuttini, P.G. Conaghan, C. Cooper, M.B. Goldring, S.R. Goldring, G. Jones, A.J. Teichtahl, J.P. Pelletier. ‘Osteoarthritis’, Nat Rev Dis Primers 2 (2016) 16072
- D. Allen, Y.M. Golightly. ‘Epidemiology of osteoarthritis: state of the evidence’, Current Opinion in Rheumatology 27(3) (2015) 276-283.
- Donell. ‘Subchondral bone remodelling in osteoarthritis’, EFORT Open Reviews 4 (2019) 221-229
- Tamaddon, L. Wang, Z. Liu, C. Liu. ‘Osteochondral tissue repair in osteoarthritic joints: clinical challenges and opportunities in tissue engineering’, Bio-Design and Manufacturing 1(2) (2018) 101-114
- F. Loeser, S.R. Goldring, C.R. Scanzello, M.B. Goldring. ‘Osteoarthritis: A disease of the joint as an organ’, Arthritis & Rheumatology 64 (2012) 1697-1707
- Castañeda, E.F. Vicente. ‘Osteoarthritis: More than Cartilage Degeneration’, Clinical Reviews in Bone and Mineral Metabolism 15(2) (2017) 69-81
- Tamaddon, S.-M. Chen, L.V. Saiz, A. Hart, M. El-Husseiny, J. Henckel, C.L. Liu. ‘Decrease in local volumetric bone mineral density (vBMD) in osteoarthritic joints is associated with the increase in cartilage damage: a pQCT study’, Frontiers in Materials 4(November) (2017) 1