Professor Eisuke Hanada from the Department of Information Science and Engineering at Saga University, Japan, explores the increasing use of e-health solutions and some of the challenges and opportunities they offer.
Applications of ‘e-Healthcare’ are expanding, and it has the potential to become an essential element of modern medicine. I believe that Information and Communication Technology (ICT) should be embraced to assist physicians in making diagnostic and treatment decisions, to help them when undertaking certain types of treatment, to assist medical staff to more clearly explain medical issues to patients, and to prevent disease. However, it must always be remembered that physicians are ultimately responsible for the medical care of their patients, and that all treatment must be under the supervision of a medical professional: these are things that cannot be delegated to a non-human.
In this article, I outline the elements of e-healthcare and what will be necessary for its development.
Hospital Information Systems (HIS) and networks
At present, patient information is, in most cases, kept electronically in computer storage devices, making it possible to input it or refer to it anywhere and at any time, as long as one has the access right. This can be achieved by utilising hospital information systems (HIS), high-speed information networks, and authentication technology to ensure security.
In recent years, systems that have enabled the distribution of patient information regionally or nationwide have been developed and have been put into operation. In Japan, the Ministry of Health, Labour and Welfare (MHLW) advocates the establishment of an environment in which patients can receive the best possible medical care by choosing a medical institution that specialises in their disease and that is fit to the severity of their condition. MHLW has named it the ‘Community Comprehensive Care Systems. To realise this system, without wasting the limited resources, it is necessary to take measures to ensure the safe sharing of patient information and the prevention of duplicate tests.
In the past, each medical institution (i.e. hospital, clinic, pharmacy) introduced its own system. To share patient information, a request letter had to be written and submitted in paper form. Even now that multiple HISs can be connected via a network, clinical data descriptions and databases are not uniform, thus common systems need to be developed that allow the sharing of data among different HISs.
In Japan, a personal identity card (‘My Number Card’) has been issued by the national government. This was designed to contain important personal information, but it has not been widely accepted by the public and cannot currently be used for medical purposes; thus patient identification cards are generally assigned by each healthcare provider, meaning that patients need a card from each of their providers to obtain service. It would be of great benefit to have a personal ID card that can be universally used. Some considerations will be necessary to ensure that people without the card, such as foreign travellers, will have better access to medical facilities.
An additional consideration of utmost importance is ensuring that patient consent be obtained before any information is collected or used. The patient should be able to control whether or not and which information is stored, used, or provided by the healthcare provider. Healthcare providers, including medical institutions and storage administrators who hold the patient’s information, must handle it in accordance with the eight principles of the OECD.
The rights to control patient information include the right to request a disclosure of information. An important issue here is that the information disclosed should be understandable to the patient; medical information, including a physician’s records, must be provided in such a way that a person with limited medical knowledge can understand it.

Technologies and issues related to e-Healthcare
Hereafter, I comment on some of the technologies that will be used to scale up e-healthcare in the future. Keywords to be considered include AI, IoT, Telemedicine, Telehealth, VR, AR, and PHR. AI and IoT were reported in a previous article, so they have not been included here.
Telemedicine and telehealth
Telemedicine has been attracting attention in Japan as a means of providing medical care to remote islands and sparsely populated areas. Japan is an island nation, and nearly 75% of its land is mountainous. The population is concentrated on the plains, as are most of the medical resources. Therefore, there are high expectations for the use of telemedicine to support medical care on our remote islands and in the mountainous areas. It has also received much attention recently as a way to more safely identify and treat patients with the COVID-19 pandemic, and its use has greatly reduced the burden on our physicians.
The resources required for telemedicine vary greatly depending on its purpose and requirements. Telemedicine must be categorised by its intended use and designed with the specific infrastructure necessary for each use. I will use the following terminology: A ‘provider’ is the physicians (doctors) who remotely performs an examination or consultation, and the ‘client’ is the patient and/or care provider who remotely requests the examination or consultation.
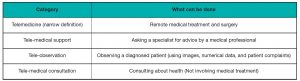
The ‘provider’ can be assumed to be a physician. Clients can be classified into three categories, as shown in Table 1.
In Japan, the law allows only physicians to perform medical treatment. Therefore, what can be done in situations other than ‘D to D’ is limited.
In addition, telemedicine can be categorised according to what is performed, as shown in Table 2.
Another possible alternative is ‘telehealth instruction’ (or ‘telehealth education’). Tele-medical instruction, in which medical practice is taught remotely, does not fit the narrow definition of telemedicine.
Applications that do not involve medical treatment are categorised as tele-health, and other cases can be classified as tele-medicine.
In Japan, if the situation in the past was not ‘D to D’, only ‘tele-medical consultation’ could be done. Recently, however, ‘tele-medical observation’ has been permitted in a ‘D to P’ situation. For tele-medical observation to be successful, all pertinent data must be carefully prepared by the patient before the consultation. Also, both parties must be equipped with and receive sufficient training in the use of devices that can process the patient’s data with sufficient accuracy that it can be trusted by the physician. Because of the COVID-19 pandemic, in Japan, MHLW revised the instructions, which is the interpretation of the law, so that physicians can, until the situation normalises, conduct medical consultations through video conferencing, even if it is the initial examination. Although it is difficult for doctors to do the initial examination without directly seeing the patient, allowances had to be made due to the situation. It is hoped that the benefits of ‘tele-medical observation’ will become apparent and lead to its increased use after the pandemic passes.
Telemedicine can be divided into two types by the method used for the handling of data: a ‘Stored & Forward’ type and an ‘Online’ type. The Stored & Forward type has already been commercialised, represented by remote radiological diagnosis (Tele-radiology). In tele-radiology, image data are transmitted from a ‘client’ to a specialist ‘provider’. The specialist reconstructs images from the data, and makes a diagnosis using the reconstructed images. In Japan, taking radiological images can be done only by licensed medical radiologists and physicians. Imaging by a medical radiologist must be done with the instruction of a physician. Remote pathological diagnosis (tele-pathology) can be done using the same procedure, and there are numerous examples. With these two types of diagnosis, there is no concern about the length of time from the request for imaging or a diagnosis to the time the results are available; the time can vary depending on the transmission speed of the networks involved and on the amount of data contained in the image. An exception is rapid intraoperative pathology, in which the data must be able to be recorded and the results accessed in real time during surgery.
Online types, on the other hand, need further classification according to their purpose. The online types use a system similar to video conferencing. In this case, there is a trade-off between the quality of the image and the capacity of the communication line (transmission rate). In addition, there is a problem of delays in communication, in video A/D and D/A conversion, and in video display. Among these, the delay in communication has been reduced considerably in recent years, but the delay caused by conversion and display cannot be reduced to zero. Based on this, I believe there are some surgeries that will be difficult to perform remotely using a digital line.
When classified in this way, it can be seen that a fast network is not necessary for the Stored & Forward type, except in a few cases. Early tele-radiology in Japan used a 32 kbps line to transmit digitised radiological images, and specialists responded with text data and compressed images. Even with only this level of infrastructure, Stored & Forward telemedicine is possible. In India, patient monitoring can be done using a satellite phone and vital signs, which are text data.
In contrast, with the online-type a communication line of at least 600 kbps is required when video is used, such as for confirmation of operation or endoscopic images. As communication lines have become faster in recent years, there is high expectation for improvements through the use of high-definition images, such as HD, 4K and 8K. However, the size of the display, the limitations of the small pixels in the display device, and the limitations of the resolution of the human eye must be considered. It is also important to note that high-definition images have an extremely large amount of data when they are stored. 5G is expected to be applied to remote surgery because of its low latency in communication lines. However, as mentioned earlier, it is not possible system-wide to achieve zero delay.
VR (Virtual Reality), AR (Additional Reality)
In VR everything in the field of view is a virtual reality, and AR is a superimposition of the virtual on reality.
In the clinical field, VR can be used in a variety of situations. The presentation of three-dimensional images of organs, which is possible using a series of CT images, can also be called VR. This technique has been used, for example, in the treatment of liver cancer, not only to present the position of the affected area in three dimensions, but also to consider the procedure for avoiding the normal part of the liver when resecting a tumour. In radiotherapy, it helps to determine the precise irradiation position using the three axes. In addition to this, when building or renovating a hospital, VR can be used not only as a drawing tool but also as a tool for the hospital staff to grasp the flow lines and distance more realistically, which helps to create a better space. For patients, the use of VR makes it possible to understand the environment from various perspectives before being admitted to the hospital. The use of VR to provide a view of the hospital before the visit can be a factor in increased patient satisfaction.
AR is expected to help people of various specialties in their actions and tasks. The results of the aforementioned studies on VR-based surgery can be used in an AR system, for example to guide the path of an endoscope. This technique is already in use in gastrointestinal and brain surgery. This guide tool has the potential to drastically improve surgical outcomes. However, because of the movement of human organs, the key is to respond to changes in time. Another use is based on the fact that patients sometimes get lost when moving between examination rooms or from their examination room to the accounting desk, especially in large hospitals. There are some examples of voice-based assistance, but I think that more reliable guidance will be possible by the use of AR.
In telemedicine, both VR and AR will allow doctors to provide more detailed explanations to patients. For example, a radiological image is currently a cross-sectional view, but a VR three-dimensional image will make it possible to explain in more detail the location and the size of the affected part of an organ. Adding to this, the use of the cloud will make it easier to provide a variety of image information through the sharing of spatial data between the telemedicine client and provider. Currently, telemedicine cannot communicate the senses of touch and smell, but by further deepening the linkage between sensor technology and VR and AR, it can be expected that more such information will be available to the client and that the scope of telemedicine will be expanded.
Personal Health Record (PHR)
PHR can be used for the sharing of health information, as I indicated in the HIS section. In order to achieve this, there is a choice between managing personal health information and information related to medical care on the individual’s own terminal or managing it in the cloud or other storage.
The information to be registered in PHR may vary greatly depending on the purpose. If the purpose is to maintain good health, this could include daily vital signs (blood pressure, heart rate, etc.), number of walking steps, amount of exercise, and calorie intake. In addition to these, information for medical use might be considered, such as blood type, allergies, pre-existing diseases, the name of the medicine the user is taking, emergency contact information, and information about the user’s medical institution.
In either case, PHR will be a collection of personal information for which due consideration to its use must be given. It is simply a matter of setting the type of information to be registered and the access rights to the individual information registered. In setting these up, the first consideration should be that the intention of the person who registered the information be respected. It should be noted, however, that access rights can also vary depending on whether or not the person is able to express their intention. When a person enters information into the PHR or references that information, the access to the PHR may be from a device such as a smartphone. In these cases, the compatibility with the security function will be a problem. It is also conceivable that the registered person may grant access to limited information or to only their personal physician, so it is easy to imagine that the management of this setting would be extremely complicated. If the person is unconscious and emergency access rights were not set up before the crisis, the registered information cannot be accessed and, as a result, life and death decisions could be affected.
When building a PHR in a cloud, the following concerns remain:
- It may be unclear where the information is actually stored; and
- Cloud administrators may be administratively entitled to see the data.
The conditions for the secondary use of personal information should also be clarified, and the consent of all users should be obtained before any changes are made.
Expectations for e-health
In this article, I described technologies and issues that I believe are relevant to e-Healthcare. The digitisation and distribution of medical information is necessary to realise so-called ‘smart’ medicine. However, over reliance on computers and networks can lead to problems with information management, especially leakage and unauthorised use.
We believe that people should be more concerned about and involved in their healthcare, considerations that can be improved by access to their personal information through ICT, based on knowledge of both the benefits of its use, and the dangers it can pose.
Professor Eisuke Hanada
Department of Information Science
and Engineering
Faculty of Science and Engineering
Saga University
+81952288586
hanada@cc.saga-u.ac.jp
www.ai.is.saga-u.ac.jp/~hanada/index-e.html
Please note, this article will also appear in the third edition of our new quarterly publication.