New research has highlighted biological and gender-driven disparities shaping antibiotic dosing, therapeutic effectiveness, and outcomes in sepsis treatment.
It also brings attention to how biological sex and gender inequities contribute to suboptimal sepsis treatment, potentially compromising outcomes for women.
Despite advances in early detection and treatment, standardised antibiotic dosing frequently ignores patient-level variability – especially that associated with sex-related physiology and gender-influenced care disparities.
The research examines the overlooked pharmacokinetic and pharmacodynamic differences between men and women, and advocates for the integration of sex and gender into antimicrobial dosing protocols.
The urgent need for improved sepsis diagnosis and treatment
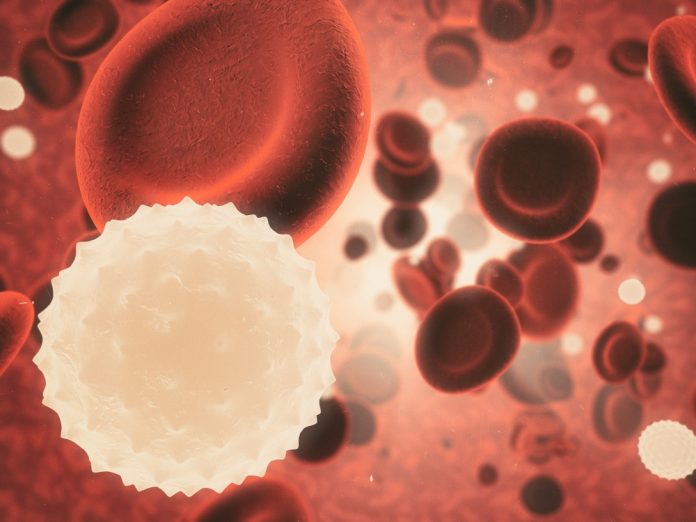
Sepsis is dangerous because it is the body’s extreme and life-threatening response to infection.
When an infection spreads and triggers a widespread immune reaction, the body releases chemicals into the bloodstream that cause inflammation throughout the body. This can damage tissues and organs, leading to decreased blood flow, hypotension, and organ failure.
If not recognised and treated quickly, sepsis can progress to septic shock, a severe form that causes dangerously low blood pressure and can be fatal. Even with treatment, sepsis can result in long-term complications such as chronic fatigue, organ dysfunction, or post-sepsis syndrome.
The condition develops rapidly, making early detection critical to survival. Prompt diagnosis and treatment with antibiotics and fluids are essential to reduce the risk of death and improve recovery outcomes.
There were gender disparities in several sepsis treatment areas
The researchers found that women often face both underrepresentation in pharmacological trials for sepsis treatment and face higher risks of antibiotic overexposure.
Hormonal fluctuations, body composition, and renal clearance all influence how drugs are processed, yet these variables are rarely considered in dosing algorithms.
Meanwhile, men – especially younger individuals with augmented renal clearance – may be underdosed, leading to treatment failure.
The authors stated: “Standard dosing overlooks key biological differences. Women, due to altered metabolism and lower muscle mass, are more vulnerable to adverse effects, while young men often eliminate drugs too quickly to maintain therapeutic levels.”
Gender roles and biases complicate how patients are cared for
Beyond biology, gender roles and biases further complicate sepsis care.
Women are less likely than men to receive aggressive or timely interventions, with disparities stemming from symptom misinterpretation, healthcare-seeking behaviours, or implicit bias within emergency systems.
These inequities exacerbate the biological differences that already influence pharmacokinetics and pharmacodynamics. Standardised dosing often overlooks how women are more prone to antibiotic overexposure and adverse reactions, while younger men with augmented renal clearance face underdosing and treatment failure.
These imbalances underscore the need to tailor antimicrobial therapy for sepsis treatment more precisely.
New protocols on the role of sex and gender in treatment needed
The authors advocate for wider use of therapeutic drug monitoring to individualise treatment and reduce both toxicity and resistance.
They also call on the scientific community to integrate sex- and gender-aware research protocols, noting that fewer than 30% of studies currently report sex-stratified data.
Professor Jordi Rello, who co-authored the study, concluded: “Understanding the differences shaped by sex and gender is essential to advancing personalised medicine and represents a commitment to reducing the equity gap.”