The route to faster results, better treatment, and improved outcomes in sepsis patients.
Sepsis is a critical and potentially life-threatening clinical syndrome representing the ultimate host immunological reaction to an invading microorganism. Sepsis is defined as a “life-threatening organ dysfunction caused by a dysregulated host response to infection” and may affect several organs.
Patients with sepsis constitute a large and very resource-demanding patient group within hospitals, and the WHO estimates in a 2020 report that the global sepsis mortality is 20% among more than 49 million cases. In the US, sepsis is the tenth leading cause of death among hospitalised patients and the most expensive to diagnose.
During 2012-2018, the annual costs of sepsis among hospitalised patients rose from $27.7bn to $41.5bn. In septic patients, time-to-coverage of antimicrobial treatment has been shown to be critical for the patient outcome, especially in severe sepsis, where the survival rate drops by 7% for every hour during the first six hours if the patient is not receiving appropriate antimicrobial treatment.
Enhancing sepsis diagnostics: The need for speed and sensitivity
Appropriate antimicrobial treatment requires knowledge of the identity and susceptibility of the invading microorganism. Initially, this is not known, and the patients are receiving empiric treatment based on clinical presentation (where the likely focus of infection is) and historical knowledge regarding the prevalence of different microorganisms in different foci and the susceptibility patterns of these microorganisms. Once the microbial identity and susceptibility pattern have been determined, the initial empirical treatment may be adjusted to targeted therapy, which in some patients will require escalation to broad-spectrum antimicrobials and in other cases may allow de-escalation to narrow-spectrum antimicrobials.
A large number of different invasive bacteria and fungi can facilitate the development of a cascade of immunological events that lead to clinical sepsis. The current diagnostic Gold Standard for a systemic infection/sepsis is blood culture, which remains negative in 50%-75% of patients with clinical sepsis. The low sensitivity, combined with a long turnaround time (typically 1-3 days from sampling to species identification, followed by an additional 18-24 hours for determination of the antimicrobial susceptibility pattern), is highly unsatisfactory for the clinical management and outcome of patients with sepsis. Faster and more sensitive diagnostics would allow clinicians to optimise individual patient treatment, likely resulting in increased survival of the individual patient as well as reduced burden of broad-spectrum antimicrobials in the population.

Potential solutions
Faster sepsis diagnostics may be achieved by either direct-from-blood molecular detection of the microbial species ID (which will not reveal the antimicrobial susceptibility pattern) or by rethinking the conventional microbial growth-based blood culture technology by including microbial catchment and enrichment steps.
Direct-from-blood molecular detection of microbial species ID was first introduced by Roche Molecular Systems (SeptiFast). However, the system, as well as several subsequent commercially available PCR-based systems for the detection of microorganisms directly from patients’ blood without prior enrichment/culture, was discontinued largely due to high costs combined with the inability of the supplier to guide clinicians on which patients should be tested. These new add-on diagnostics are very expensive – so expensive that they cannot be offered to every patient who is being blood cultured.
With no clear guidance on how to select patients, no one will be selected. The current selection process for microbial ID and susceptibility testing for microorganisms present in the bloodstream is blood culture itself. However, some 90% of cultures do not grow, but this takes 3-5 days to determine. Faster yet cost-effective patient selection and subsequent diagnostics are required for patients needing urgent results.
Additionally, particularly for susceptibility tests requiring viable microorganisms, a rapid, low-cost selection and enrichment method for viable organisms is warranted.
A new approach
There is a solution: AI-based selection of high-risk patients that will have the highest potential for obtaining a benefit that may pay for the cost of the new (and expensive) add-on sepsis diagnostic test.
The optimal approach would be the capability to select high-risk patients for the new add-on diagnostic test at the time of obtaining a patient’s blood sample for blood culture testing. Such a selection must fulfill the following requirements:
- Be fast and easy to perform (minutes) without expert knowledge of infectious diseases.
- Be reproducible.
- Be based upon available information (initial patient examination and/or initial tests).
- Be able to identify a subgroup of patients that will have a substantially higher positive rate in blood culture compared to the average positive rate for all patients receiving a blood culture.
- Avoid exclusion of patient groups with a high positive rate in blood culture.
By only providing the new (and expensive) diagnostic test to a subgroup of the whole ‘blood cultured’ patient population, most benefits will still be achieved, but the costs will be significantly reduced. The precise cost/benefit ratio improvement will depend on the reduction of costs (the size of the subgroup compared to the whole group) as well as the reduction of the benefits (how well the subgroup is identified – i.e., how well the benefits are retained). This information is currently unavailable and awaits future randomised clinical intervention and outcome trials.
SepsiSTAT: A potential cost-effective alternative to blood culture with ID and susceptibility in less than 12 hours
As Dr Lisby makes clear, sepsis is fast, deadly, and expensive to treat. Blood culture-based diagnosis is relatively inexpensive but has insufficient sensitivity and a too-long time-to-result in patients with sepsis. So far, faster diagnosis methods have proved too expensive to be used on all suspected patients.

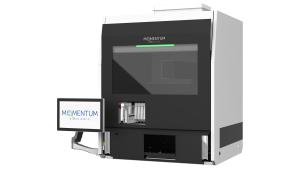
Momentum’s solution to these difficulties is an automated system, SepsiSTAT®, that potentially can do what blood culture does now but in far less time – typically 4-8 hours instead of 18-36 hours for positives, or five days to confirm a negative. This adds to the rapid selection process Dr Lisby described, post- Sin-silico/AI selection. Positive samples can be tested by routine ID and susceptibility methods already used for blood culture isolates. The system also has several features in addition to conventional blood culture:
- Automated isolation and concentration of blood specimens into purified culture.
- Integral reporting of Gram-positive bacteria/Gram-negative bacteria/ yeast at the same time as reporting detection.
- Monitored growth to one or more defined microbial concentrations for direct application of output to other ID/susceptibility/sequencing systems.
SepsiSTAT is the result of seven years’ work funded by investors and grants, notably a £2.5m Horizon EIC Accelerator/Innovate UK grant developing the automated prototypes now running in Momentum’s laboratories. Our small but dedicated team is now based at Milton Park in Oxfordshire.
For more information, please visit the Momentum Bioscience Website.
Disclaimer
Jan Gorm Lisby is the Chief Physician at the Department of Clinical Microbiology, University of Copenhagen, Hvidovre Hospital, Kettegaard Alle 30, DK-2650 Hvidovre, Denmark. Dr Lisby is a paid advisor to Momentum Bioscience Limited.
Please note, this article will also appear in the 22nd edition of our quarterly publication.