The FEMaLe project is working on realising a Machine Learning multi-omics platform that can analyse omics datasets and feed the information into a personalised predictive model.
European healthcare systems are under pressure from megatrends, including an increasingly ageing population. This means that a growing number of people are confronted with having often multiple chronic conditions.
In addition, they are faced with the lack of coherent monitoring, collection, and data usage to support clinical decisions and treatments, reducing patient adverse events, diagnostic delay, misdiagnosis, or lack of a diagnosis altogether.
As a result, systems are currently responsive rather than preventive.
Without any action towards personalised early risk prediction, prevention, and co-ordinated intervention, systems will face many more patients suffering from chronic diseases. This includes multimorbidity, reducing quality of life and causing healthcare costs to rise.
The ongoing ‘Finding Endometriosis using Machine Learning’ (FEMaLe) project builds upon the report from the European Commission (EC) on State of Health in the European Union (EU), which argues that prevention and primary care are the two major priorities in this decade.
Preventive responsive actions to people suffering from diseases, including endometriosis, will greatly optimise quality of life and reduce healthcare costs, e.g., through fewer surgeries, hospitalisations, and rehabilitation programmes.
Detailed clinical and psychosocial phenotyping of people with endometriosis, transformed into clinical decision support tools, could be a first step towards achieving earlier detection, avoiding unnecessary laparoscopies. Just imagine if endometriosis could be correctly diagnosed sooner and treated to bring this burden down – not only for those affected by endometriosis, but also for society in general.
The FEMaLe project will develop and validate a Machine Learning (ML) multi-omic platform that can convert population datasets, phenotypic and genotypic, into a comprehensive and personalised predictive model to improve intervention along the continuum of care for people with endometriosis.
Endometriosis: The last health taboo
The World Health Organization (WHO) recognises the importance of endometriosis and its impact on people’s sexual and reproductive health, quality of life, and overall wellbeing. Endometriosis affects approximately one in ten (190 million) women and people assigned female at birth worldwide.
It is a chronic condition marked by the presence of endometrial-like tissue outside the uterus, which in many patients is associated with debilitating and painful symptoms. It takes an average of 7.5 years from the onset of symptoms to diagnosis, which has a negative impact on health-related quality of life.
Patients with endometriosis are also at greater risk of infertility, emergence of fatigue, multisite pain, and other comorbidities. Thus, endometriosis can negatively affect every aspect of a patient’s daily life, including sexual relations, appetite, exercise, sleep, emotional wellbeing, social activities, childcare, and work and household productivity.
The ‘EndoCost Quality of Life Study’ demonstrated that the average annual healthcare costs are three times higher for people with endometriosis compared with people without, even five years before and five years after diagnosis. The total workplace productivity loss averages 11 hours per week, with most of that loss caused by presenteeism.
Endometriosis affects people during the prime years of their lives – a time when they should be finishing education, starting and maintaining a career, building relationships and having a family.
Despite high prevalence and costs, endometriosis remains underfunded and under-researched, greatly limiting our basic understanding of the disease, and slowing much-needed innovation in diagnostic and treatment options.
The FEMaLe project
The FEMaLe H2020 project is a European project with international impact, driven by megatrends (increasingly ageing population, unharnessed health data value creation, and diagnostic delay), seeking to deliver a comprehensive model for personalised early risk prediction, prevention, and intervention for people with endometriosis, based on state-of-the-art Big Data technologies.
Complex diseases, such as endometriosis, are driven by multiple networks of interconnected causative factors and metabolic processes. Patients’ disease risks, rate of progression, and responses to therapy vary due to combinations of their mutations, predisposing phenotypic features, and environmental influences.
A brand-new generation of Machine Learning and multifactorial data analytics methods are enabling the FEMaLe project to start untangling the disease risk, progression, and therapy response signatures inherent in large population datasets.
Ultimately, the FEMaLe project will develop and demonstrate more clinical decision support tools, based on high-resolution stratification of people with endometriosis and Deep Learning in medical imaging to enable non-invasive diagnostics.
Stratifying patient populations
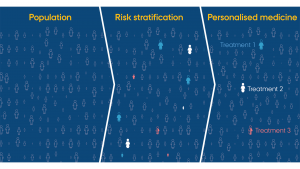
Improvements in analytical methods enable the disentangling of complex diseases into distinct patient subgroups that have different root causes and influences, as proposed by PrecisionLife, a UK-based pioneering techbio company.
The key to understanding diseases at a deeper level is to find combinations of these factors (disease signatures) that distinguish one patient subgroup from another. This provides a more granular way of segregating patients, giving a higher-resolution view of the disease and opportunities to treat subgroups of patients with better, more personalised precision medicines.
Analysing Danish and UK biobank data with the PrecisionLife combinatorial analytics platform recently achieved two firsts in endometriosis:
- Genetic risk factors were identified to classify women as being at high or low risk of developing endometriosis; and
- Patients with endometriosis were stratified into genetic subgroups to provide insight into potential new drug targets and drug repurposing opportunities to accelerate the development of effective treatments at reduced risk and cost.
The results of this analysis were presented at the 15th World Congress on Endometriosis in May 2023 and are intended to be submitted to peer review later this year.
Augmented Reality to real-time guide surgeons
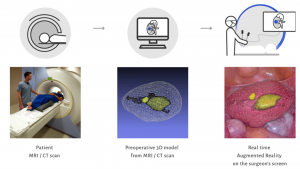
Laparoscopy has brought considerable changes to all fields of surgery by introducing the concept of minimal invasive surgery. It is the most common procedure to both diagnose and remove mild to moderate endometriosis. Laparoscopy has not only revolutionised the approach in surgery; it has substantially improved the surgeon’s vision.
The next revolution is Augmented Reality (AR), and a core FEMaLe feature is to introduce AR in laparoscopic surgery in hospitals, led by French start-up SURGAR (Surgical Augmented Reality).
The FEMaLe project will create an AR tool, based on Big Data and Machine Learning, to real-time guide surgeons in the laparoscopic operation of endometriosis by visualising the endometriosis lesions and suggesting the division plane to the surgeon – a task that requires years of experience. This will be achieved through collection and annotation of Big Data, using computer vision and Machine Learning techniques to learn from video data.
The AR tool aims at improving the outcome of surgeries by adding an overlay over suspected lesions, along with predicted class. That will allow for reducing the risk of missed lesions, especially for junior surgeons, enabling more effective, accurate and efficient surgical procedures.
By developing this next-level AR tool, FEMaLe aims at standardising the surgical operations on endometriosis, enabling the junior surgeons to experience a better operation for the benefit of patients’ health and safety. Utilising the AR tool, a new and common vocabulary between surgeons and machines could be established.
This will be achieved using multiple Deep Learning approaches, based on artificial neural networks, complying with the EC guidelines on trustworthy AI which should be lawful, ethical, and robust. For Deep Learning to succeed, good data is needed which means that, on the collected laparoscopy video data, certified surgeons must annotate the division plane.
Since the intra-surgeon variability is high due to a lack of standard techniques, the data will be qualified and reviewed several times to establish ethical and robust data. Based on this large amount of high-quality annotated data, the machine can be trained and taught to suggest the division area.
Finally, the algorithm will be integrated into SURGAR software, enabling real-time guidance to assist the surgeon in finding the division planes around the lesion.
Citizen health science using modified Lucy app
The FEMaLe project uses a citizen health science approach to empower endometriosis stakeholders from passive recipients of services to engaged change agents.
FEMaLe will safely collect patient data through the modified Lucy app, an advanced period tracker developed by Hungarian start-up Codingo, and feed resulting endometriosis risk scores and other health recommendations back to its users. This can facilitate much-needed shared decision making in primary and secondary care, contributing to patient empowerment and a more personalised pathway, based on increased health literacy, and raised awareness on endometriosis.
Data collected from the Lucy app reveals more participation from patients with endometriosis than from those without, indicating strong engagement and willingness to help address the last health taboo. The Lucy data corroborates clinical results through lived experiences, but it also highlights interesting patterns in food consumption, physical activity, and experiences of pain.
However, this analysis needs to be further validated in a larger group of patients. Cutting-edge techniques have been used to deal with the sparsity, noise and irregularity of patient data which needs further development.
We are FEMaLe
The FEMaLe consortium is composed of a total of 17 partners from nine countries (Denmark, Hungary, the UK, France, Latvia, Sweden, Turkey, Norway, and Serbia). Each partner has been carefully selected based on the most accurate endometriosis expertise and experience for all the intended outcomes and proposed objectives.
FEMaLe is structured around a healthcare-related partnership at a different level and position of the value chain. It is co-ordinated from the Department of Public Health at Aarhus University in Denmark.
The endometriosis market and FEMaLe’s impact
The global endometriosis market is forecast to reach $2.42bn by 2026, according to a report by Reports and Data. The endometriosis market held a market share of $1.93bn in the year 2018, and it is forecast to grow at a rate of 2.8% until 2026.
Rising incidences of endometriosis mainly due to an increasing population within the age group of 15-49 years across developed and developing economies, diagnostic improvements leading to early identification, environmental factors, and rising awareness are the key factors contributing to growth of the market.
North America dominated the global endometriosis market in 2017 and is expected to grow at a lucrative compound annual growth rate (CAGR) by 2025. High prevalence within the US has created a potential market for drug manufacturers.
Asia Pacific is projected to witness the fastest growth rate of 5.5% during the forecast period and occupied the second-largest market share of 24.3% in 2018.
Europe also occupies a prominent market position, resulting from the continuous growth of the healthcare sector and rising investment in the industry. The FEMaLe project paves the way for new minimal invasive surgery with major impacts on surgical healthcare systems worldwide and improved life quality for the patients.
Also, most recent major FEMaLe developments within stratification of patients with endometriosis into genetic subgroups offers huge innovation potential in diagnostics and treatment regimes, including the novel drug discovery, a selection of therapies that are more closely targeted at patient subgroups, and ultimately the delivery of more personalised care to patients.
 This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 101017562.
This project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 101017562.
Disclosure: The present document reflects only the author’s views, and the European Commission is not responsible for any use that may be made of the information it contains.
Please note, this article will also appear in the fifteenth edition of our quarterly publication.









