Atomic physicists and nuclear medicine experts at the University of Tokyo and the National Institute of Radiological Sciences (NIRS) have devised a simple way to characterise tumours using standard medical imaging technologies.
The Japanese team has designed a timer that can modify medical imaging technologies, such as positron emission tomography (PET) scanners, to detect the oxygen concentration of tissues throughout patients’ bodies. These findings may lead to further improvements in cancer treatments, by allowing medical professionals to quickly identify parts of tumours with more aggressive cell growth.
“Patients’ experience in this future PET scan will be the same as now. Medical teams’ experience of conducting the scan will also be the same, just with more useful information at the end,” said nuclear medicine physician Dr Miwako Takahashi from the NIRS, a co-author of the research publication in Communications Physics.
Studying positron decay in patients
Positrons are positively charged antimatter forms of electrons. Due to their tiny size and extremely low mass, positrons pose no danger in medical imaging technologies. Positrons produce gamma rays, which are electromagnetic waves similar to X-rays, but with shorter wavelengths.
First author Professor Kengo Shibuya from the University of Tokyo Graduate School of Arts and Sciences and his colleagues developed a life expectancy chart for positrons using a miniaturised PET scanner to time the formation and decay of positrons in liquids with known concentrations of oxygen.
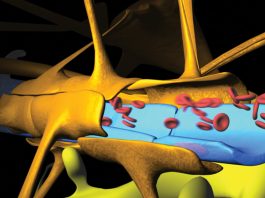
The research team revealed that when oxygen concentration is high, the positrons immediately collide with an electron and produce gamma rays. Researchers predict that their technique will be able to detect the absolute oxygen concentration in any tissue of a patient’s body based on the lifetime of positrons during a PET scan.
The team detect the lifetime of positrons using the same gamma-ray detectors that medical imaging technologies already use. Co-author, Professor Taiga Yamaya, leader of the Imaging Physics Group at the NIRS, predicts that the majority of work to transfer this research from the lab to hospitals will be on upgrading gamma-ray detectors and software so that the gamma-ray detectors can record not just location, but accurate time data as well.
Applying this research to cancer treatment
Medical experts have long understood that low oxygen concentrations in tumours can impede cancer treatment for two reasons: First, a low oxygen level in a tumour is often caused by insufficient blood flow, which is more common in fast-growing, aggressive tumours. Secondly, low oxygen levels make radiation less effective because the cancer cell-killing effects of radiation treatment are achieved by the radiation energy converting oxygen present in the cells into DNA-damaging free radicals. Thus, detecting the concentration of oxygen in body tissues would inform medical experts how to effectively attack tumours inside patients.
“We imagine targeting more intense radiation treatment to the aggressive, low-oxygen concentration areas of a tumour and targeting lower-intensity treatment to other areas of the same tumour to give patients better outcomes and less side effects,” said Takahashi.