Did you know that T cell recruiting immunotherapies with BiTEs and CAR T cells could revolutionise cancer immunotherapy?
In the future, various immunotherapeutic treatment platforms will be combined with other immunotherapy approaches, Dr Marion Subklewe of University hospital in Munich, Germany tells us more.
Towards cancer immunotherapy
Novel T cell recruiting immunotherapies such as the CD19 specific chimeric antigen receptor (CAR) T cell products Axicabtagene-Ciloleucel (Axi-cel) and Tisagenlecleucel (Tisa-cel) as well as the Bispecific T cell engager (BiTE) Blinatumomab expand the armamentarium of Cancer Immunotherapy for the treatment of relapsed and refractory (r/r) B-cell malignancies. Even though both strategies have shown unforeseen clinical success for heavily pre-treated patients in pivotal trials, T cell recruiting immunotherapies can induce potentially severe immunotoxicities such as Cytokine Release Syndrome (CRS), Neurotoxicity (ICANS) and prolonged Cytopenia.
However, continuous state-of-the-art education of treating physicians and nursing staff enables the safe application of these treatments. Here, we give an overview of T cell recruiting therapies applied at our centre, their mode of action and pivotal clinical trial data. Additionally, we outline the strategies implemented at our centre to mitigate and manage potential immunotoxicities of CD19-directed therapies.
Finally, we give a short overview of innovative next generation immunotherapies currently in development at our centre including bifunctional antibody constructs, adapter CAR T cells, combinatorial approaches with double checkpoint inhibition and hypomethylating agents as well as Dendritic Cell vaccination.

Mode of action
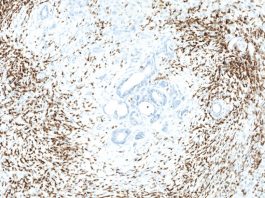
BiTEs are recombinant fusion proteins consisting of two different antibody derived single chain variable fragments (scFv). One scFv targets the T cell surface molecule CD3, while the second scFv is directed against a tumour-specific antigen. Upon binding of both targets, BiTEs link the patients’ T cells to tumour cells, which results in T cell activation and lysis of the tumour cell.1
In contrast to BiTEs, which can be applied as ‘off the shelf’ reagents, CAR T cells are individually produced for each patient. Autologous T cells are genetically modified in vitro by retroviral or lentiviral transfection to express a CAR, which enables the activation of the T cell when binding the respective tumour specific target. CARs are synthetic receptors containing an extracellular tumour antigen specific scFv, a transmembrane hinge and spacer domain and intracellular components of the T cell receptor (TCR). In contrast to the conventional TCR, the extracellular tumour-specific scFv enables the MHC-unrestricted antigen recognition. Upon antigen binding, the intracellular CAR components (costimulatory domains and CD3ζ-chain) lead to the activation of the CAR T cell, which then releases tumour lytic proteases and cytokines and finally destroys the target cell.2
In contrast to all ‘conventional’ drugs (including BiTEs), autologous CAR T cells proliferate upon activation in the patient and are able to be persistent (even as memory-like T cells) over a long period of time, thereby facilitating long lasting immunity against the malignancy.
CAR receptors of currently approved CAR T cell products (Axi-cel and Tisa-cel) comprise one intracellular costimulatory domain and belong to the so-called second generation of CAR T cells (first generation CAR constructs did not incorporate any costimulatory domains and widely lacked efficacy in inducing an anti-tumour response). Current research investigates the potential of future CAR generations with different combinations of costimulatory domains or the ability of cytokine secretion for a more potent activation and sustained persistence of the CAR T cells.3-5
All currently commercially available T cell recruiting immunotherapies target CD19, as CD19 is not expressed on hematopoietic stem cells but on all stages of B cell maturation and, thus, on most B cell malignancies. In addition, resulting B cell aplasia as an on-target-off-tumour toxicity is manageable with immunoglobulin substitution.6,7 However, other target antigens like BCMA (B-cell maturation antigen) are also explored in clinical trials, e.g. for immunotherapy of multiple myeloma.8 We expect to see BiTE and CAR T cell constructs targeting other antigens (not only for the treatment of hematologic, but also for solid malignancies) to enter into clinical trials in the near future.
Clinical trials
T cell recruiting immunotherapy has been shown to be highly efficacious in the treatment of relapsed/refractory (r/r) B cell neoplasms. Blinatumomab has been approved for the treatment of r/r B-cell precursor Acute lymphoblastic Leukemia (BCP-ALL) following results of the phase III TOWER trial. In that trial, Blinatumomab was able to induce significantly higher response rates compared to standard-of-care chemotherapy (44% vs 25%).
Progression-free rate at six months (31% vs 12%) and median overall survival (7.7 vs 4.0 months) was also significantly improved with Blinatumomab.9 Blinatumomab treatment has also been shown to be highly successful in patients with persistent or relapsed measurable residual disease (MRD), with MRD conversion rates after one cycle of therapy of up to 78%.10
The clinical phase I-II trials ZUMA-1 (NCT02348216) and JULIET (NCT02445248) showed an overall response rate (ORR) of 52 – 83% with a complete remission (CR) rate in 55 – 58 % of the heavily pretreated patients and led to the approval of Axi-cel and Tisa-cel for relapsed or refractory (r/r) large B-cell lymphoma.11,12 During a longer follow-up period of 14 – 27 month, 30–37 % of the patients showed a sustained remission.12,13 Within the pivotal ELIANA trial (NCT02435849, n = 30) 90% of the peadiatric BCP-ALL patients achieved a CR.14 In a smaller cohort of adult BCP-ALL patients, the median overall survival was 12.9 months after treatment with anti-CD19-CD28-CD3 ζ CAR T cells.15
Lisocabtagene-Maraleucel (JCAR017, Liso-cel) is currently being investigated as another CD19-specific CAR T cell product in clinical trials. Liso-cel incorporates a 4-1BB costimulatory domain and is administered in a defined CD4:CD8 ratio of CAR T cells (TRANSCEND-NHL-001, NCT02631044). Results of the pivotal trial (n = 269 treated patients) show an ORR of 73% with a CR rate of 53%, whereas rates for toxicity were surprisingly low (Grade 3 CRS in 1%, Grade 3 ICANS in 10 % of patients, (Abramson JS 2019). Currently recruiting clinical studies randomize Anti-CD19 CAR T cells against standard of care (usually high-dose chemotherapy, followed by autologous stem cell support) in earlier lines of therapy (e.g. second-line treatment of patients with first relapse of DLBCL, ZUMA-7, NCT03391466; BELINDA, NCT03570892; TRANSFORM, NCT03575351).
In addition, efficacy of CAR T cell-based treatments approaches with Checkpoint-Inhibitors or the sequential application of CAR T cells and BiTEs emerge as new treatment options in several clinical trials for patients with disease progression after CAR T cell therapy (ZUMA-6, NCT02926833; PORTIA, NCT03630159;.16

Immuntoxicity: Cytokine Release Syndrome (CRS)
CRS is the most commonly observed side effect of T cell recruiting immunotherapies and normally occurs during or shortly after initiation of the BiTE infusion or within the first week after CAR T cell therapy (93% of patients within the ZUMA-1 trial, 100% of patients within the ELIANA trial). The clinical presentation of CRS is similar to sepsis with fever, potentially complicated by hypoxia and hypotension, and resulting organ toxicities (e.g. acute kidney injury). CRS is caused by the massive release of different cytokines such as TNF-α, IFN-γ, IL-1β, IL-2 und IL-6 by highly activated (CAR-) T cells and bystander cells (e.g. monocytes, endothelial cells). IL-6 has been identified as a central mediator of the cytokine cascade, which has led to the approval of the IL-6 neutralizing antibody Tocilizumab for the treatment of CAR T cell associated CRS.
Incidence and severity of CRS has been correlated with tumour burden prior to CAR T cell transfusion in some clinical studies. A negative impact of CRS or treatment with Tocilizumab either on the response rates or the durability of response of BiTEs or CAR T cells has not been shown so far ).17 While most patients respond to Tocilizumab, a minority of patients requires the application of corticosteroids. However, those should be used restrictively, as the assumed resistance of CAR T cells against the T-cell lytic effect of steroids has not been proven yet and a potential negative effect on the long-term treatment outcome is unknown.18
Neurotoxicity: Immune effector Cell Associated Neurotoxicity Syndrome, ICANS
Neurotoxicity is less often observed than CRS and is more frequently observed with CAR T cells than with BiTEs (67% of patients within the ZUMA-1 trial, 65% of patients within the ELIANA trial). In most cases ICANS starts after the onset of CRS. A later onset such as weeks after CAR T cell transfusion has been described in few patients. Neurological symptoms can range in severity from difficulties in speaking and writing and mild tremors to seizures, loss of consciousness or cerebral edema.
Some rare fatal cases of ICANS have been reported, but symptoms are reversible within days in most cases.19-21 High tumour burden, higher CAR T cell expansion and the treatment with anti-CD19-CD28CD3ζ CAR T cells have been correlated with a higher risk for ICANS. In contrast to CRS a central mediator as a potential therapeutic target has not been identified yet. Hence, higher grades of neurotoxicity are managed with corticosteroids.22
Taken together, the management of patients receiving T cell recruiting immunotherapies requires specifically trained medical and nursing staff. Patients are treated by a team of dedicated physicians with extensive experience in the treatment of patients with CAR T cells and BiTEs. Patients are treated on an intermediate care unit with centralised monitoring facilities, with nursing staff also specifically trained to recognise toxicities in early stages. We are involved with the design of national and international guidelines for patients receiving T cell recruiting immunotherapy and participate in clinicals trials for a multitude of indications to offer the most cutting-edge treatment options to our patients. To improve the management of patients treated with BiTEs & CAR T, we have developed an app called ‘MyTcells’ to support, guide and educate medical staff in dealing with immune-related adverse events like CRS, ICANS, HLH and pancytopenia.
Further activities at our center
We are continuously exploring novel target antigens for antibody based and CAR T cell approaches. Utilising flow cytometry, proteomics and mass spectrometry, we validate known target antigens and explore novel target structures. We have advanced current constructs by generating dual specific antibody constructs that rely on targeting of a tumour-associated antigen and blocking an innate or adaptive inhibitory checkpoint molecule.23
Novel target antigen combinations for targeting various hematological diseases are being explored by an adaptor CAR T system to increase specificity and decrease toxicity. Preclinical studies are the rational for conducting a phase I/II trial utilising dual checkpoint inhibition in combination with hypomethylating agents in acute Leukemia. Lastly, we have finished a dendritic cell vaccination trial in patients with high risk AML.
We perceive that in the future various immunotherapeutic treatment platforms will be combined with other immunotherapy approaches or in conjunction with small molecules. This work is done at the LMU-Gene Center in Munich in close conjunction with the Hematology & Oncology department at the Klinikum of the University of Munich.
References
- Kohnke, T., Krupka, C., and Tischer, J. et al. 2015. Increase of PD-L1 expressing B-precursor ALL cells in a patient resistant to the CD19/CD3-bispecific T cell engager antibody blinatumomab. J Hematol Oncol 2015; 8:111
- Lim, W.A., and June, C.H. 2017. The Principles of Engineering Immune Cells to Treat Cancer. Cell 2017; 168:724-40
- Drent, E., Poels, R., and Ruiter, R. 2019. Combined CD28 and 4-1BB Costimulation Potentiates Affinity-tuned Chimeric Antigen Receptor-engineered T Cells. Clin Cancer Res 2019; 25:4014-25
- Pegram, H.J., Lee, J.C., and Hayman, E.G. 2012. Tumor-targeted T cells modified to secrete IL-12 eradicate systemic tumors without need for prior conditioning. Blood 2012; 119:4133-41
- Sadelain M., Riviere, I., and Brentjens, R. 2003. Targeting tumours with genetically enhanced T lymphocytes. Nature Reviews Cancer 2003; 3:35-45
- Hill, J.A, Giralt, S., and Torgerson, T.R. 2019. CAR-T – and a side order of IgG, to go? – Immunoglobulin replacement in patients receiving CAR-T cell therapy. Blood Rev 2019; 38:100596
- Uckun, F.M., Jaszcz, W., and Ambrus, J.L. et al. 1988. Detailed studies on expression and function of CD19 surface determinant by using B43 monoclonal antibody and the clinical potential of anti-CD19 immunotoxins. Blood 1988; 71:13-29
- Raje, N., Berdeja, J., and Lin, Y. et al. 2019. Anti-BCMA CAR T-Cell Therapy bb2121 in Relapsed or Refractory Multiple Myeloma. New England Journal of Medicine 2019; 380:1726-37
- Kantarjian, H., Stein, A., and Gokbuget, N. et al. 2017. Blinatumomab versus Chemotherapy for Advanced Acute Lymphoblastic Leukemia. New England Journal of Medicine 2017; 376:836-47
- Gokbuget, N., Dombret, H., and Bonifacio, M. et al. 2018. Blinatumomab for minimal residual disease in adults with
B-cell precursor acute lymphoblastic leukemia. Blood 2018; 131:1522-31 - Neelapu, S.S., Locke, F.L., and Bartlett, N.L. et al. 2017. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N Engl J Med 2017; 377:2531-44
- Schuster, S.J., Bishop, M.R., and Tam, C.S. et al. 2018. Investigators J. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. New England Journal of Medicine 2018
- Locke, F.L., Ghobadi, A., and Jacobson, C.A. et al. 2018. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncology 2018
- Maude, S.L, Frey, N., and Shaw, P.A. et al. 2014. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med 2014; 371:1507-17
- Park, J.H., Riviere, I., and Gonen, M. et al. 2018. Long-Term Follow-up of CD19 CAR Therapy in Acute Lymphoblastic Leukemia. New England Journal of Medicine 2018; 378:449-59
- Schuster, S.J., Bartlett, N.L., and Assouline. S. et al. 2019. Induces Complete Remissions in Poor Prognosis Non-Hodgkin Lymphoma Patients, Including Those Who Are Resistant to or Relapsing After Chimeric Antigen Receptor T-Cell (CAR-T) Therapies, and Is Active in Treatment through Multiple Lines. Blood 2019; 134:6
- Gardner, R., Ceppi, F., and Rivers, J. et al. 2019. Preemptive Mitigation of CD19 CAR T Cell Cytokine Release Syndrome Without Attenuation of Anti-Leukemic Efficacy. Blood 2019
- Davenport, A.J., Cross, R.S., and Watson, K.A. et al. 2018. Chimeric antigen receptor T cells form nonclassical and potent immune synapses driving rapid cytotoxicity. Proc Natl Acad Sci U S A 2018; 115:E2068-E76
- Karschnia, P., Jordan, J.T., and Forst, D.A. et al. 2019. Clinical presentation, management, and biomarkers of neurotoxicity after adoptive immunotherapy with CAR T-cells. Blood 2019
- Neelapu, S.S., Tummala, S., and Kebriaei, P. et al. 2018. Chimeric antigen receptor T-cell therapy – assessment and management of toxicities. Nat Rev Clin Oncol 2018; 15:47-62
- Torre, M., Solomon, I.H., and Sutherland, C.L. et al. 2018. Neuropathology of a Case With Fatal CAR T-Cell-Associated Cerebral Edema. J Neuropathol Exp Neurol 2018; 77:877-82
- Lee, D.W., Santomasso, B.D., and Locke, F.L. et al. 2019. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol Blood Marrow Transplant 2019; 25:625-38
- Herrmann, M., Krupka, C., and Deiser, K. et al. 2018. Bifunctional PD-1 x aCD3 fusion protein reverses adaptive immune escape in acute myeloid leukima. Blood (2018) 132 (23): 2484-2494
Professor Dr Marion Subklewe
Medizinische Klinik III
+49 (0)89 4400 73133
marion.subklewe@med.uni-muenchen.de
CART@med.uni-muenchen.de
Please note, this article will also appear in the first edition of our quarterly publication, the Innovation Platform.