Dr Jochen Salber, of the Knappschaftskrankenhaus Bochum, tells us about arthroplasties: the only effective therapy for patients suffering from advanced osteoarthritis.
It is estimated that the number of patients older than 60 years belonging to this disease entity will have strongly increased by 2050. Here, Salber, senior physician of the University Hospital Knappschaftskrankenhaus Bochum, Germany explores the treatment options of total joint arthroplasties and total hip arthroplasty available for those living with osteoarthritis.
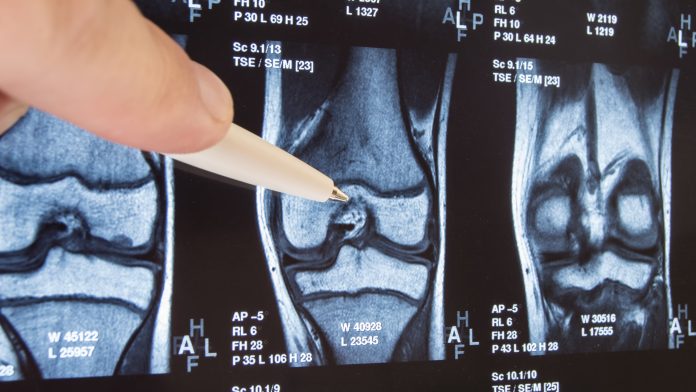
Osteoarthritis and arthroplasty
The triumphal procession of modern arthroplasty since its first prototype developed by Sir John Charnley is still indisputable. Following statistics, only this description seems to be correct however this story of success in biomaterials-based medicine also has some serious disadvantages.
Total joint arthroplasty (TJA) and total hip arthroplasty (THA) are the only two effective choices available for patients suffering from an advanced degenerative arthropathy, also known as ‘osteoarthritis’ (OA), of the affected joint (such as the hip). Primarily affecting older adults, the OA of the hip is one of the most prevalent diseases of the musculoskeletal system and is one of the main reasons for restricted mobility accompanied by pain and vice versa. Data investigated and published (2018) by the World Health Organization (WHO) indicates that around 12% male and 20% female patients older than 60 are suffering from OA symptoms, with approximately 30% considered as being severely disabled.1
It is estimated that the number of patients older than 60 years belonging to this disease entity will have strongly increased by 2050. Therefore, with the aging world population, more modern orthopaedic implants, also called joint endoprosthesis, will become increasingly more necessary every year. Statistics are demonstrating that the number of THAs (and of TJAs in general) has continuously increased over the past 10 years. The highest numbers in EU Member States are in Austria and Germany reaching around 300 THAs per 100,000 citizens. This number is closely followed by Sweden, Denmark and France with around 200 hip joint endoprosthesis per 100,000 citizens.2
Therefore, the advantages provided to OA patients by modern orthopaedic implants in terms of reduction of pain, preservation or reconstitution of mobility, and improvement of quality of life are incontrovertible, but this triumphal procession also has a dark side.
What does this mean?
These highly selective types of operations are generally considered routine and the two most frequently applied orthopaedic surgeries are THA and total knee arthroplasty (TKA), both showing an approximate mean durability of 15 years (more specified N(THA) > N(TKA) with N = “the number of”) with a high success rate. Nevertheless, every first endoprosthesis implantation and particularly the second, are bearing complications statistically in the range of 0.5 – 1.0% for THA and 0.5 – 2.0% for TKA. The two most often occurring complications after the first THA are periprosthetic osteolysis (PPOL), subsequently resulting in aseptic loosening (34.4%) and microorganisms-derived periprosthetic infections (PPI) with finally occurring septic loosening (18.9%) based on 2018 data of the German ‘EPRD’ arthroplasty register.3 In comparison, up to 40,000 hip arthroplasties need to be revised each year in the US and 30,000 in Germany.3,4
Although the complication rates may not seem very high, from an individual patient’s point of view who is suffering from one or both of these complications, their life will become a nightmare (not to mention all the socioeconomic aspects and impacts). Both types of complications are two different disease entities with different causes and pathomechanisms, therefore here only one of both will be discussed pathomechanistically in more detail, the PPOL with resulting aseptic loosening. Additionally, a novel approach will be presented with the intention to make revision THAs after AL more successful in terms of enhancement of their lifetime.
What are the reasons for PPOL and AL?
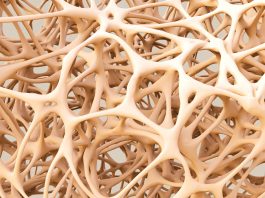
Based on our current knowledge, different aspects are responsible for triggering a PPOL and finally an AL leading to a necessary revision of the implant. Apart from patient specific reasons, further risk factors are implant-dependent and a various surgical factors. Focusing the types of currently used orthopaedic implants in THA and the biomaterials they are made of, two key triggers are wear debris micro- and nanoparticles (metal-metal, ceramic-metal, polyethylene (PE)-metal, PE-ceramic and ceramic-ceramic) and metal ions – both of which are released from the mobile parts of the THA implants into the surrounding tissue microenvironment. These degradation products generated by mechanical wear and electrochemical corrosion are not inert as former findings have suggested. Although wear rates by electrochemical corrosion have been drastically reduced and implant biomaterials have been continuously improved, lower local concentrations are still suspected to interact with the surrounded host tissue and with specific cells of the inate immune system (specifically macrophages and dendritic cells) at the biointerface – the interface between the foreign materials and the host’s biology.
The macrophages are not locally fixed within the surrounding connective tissue of the articular neo-capsule, they are able to actively interact with their microenvironment and occupy the capabilities of acting and reacting (e.g. mechano- and chemosensing, migrating, and phagocyting by endocytosis). In this context, macrophages are moving around and phagocyte foreign material – such as the mentioned wear particles (e.g. PE particles smaller than 2-3 µm2) and metal ions (i.e. different oxidation states of metals like titanium, iron, cobalt, chromium, and molybdenum). Once the foreign material is engulfed and digested a series of biologic reactions occur, such as the activation of T-cells through antigen presentation, release of pro-inflammatory mediators, cytotoxicity, DNA damage, and oxidative stress.
In 2005, the mechanism of this non-pathogenic-driven activation of innate and adaptive immunity has been unravelled.5,6 This pathway was named “inflammasome” and the activating stimuli: “danger associated molecular patterns”. The inflammasome complex of proteins was the first pathway to explain how cells transduce sterile, nonpathogen-derived stimuli (particles), into an inflammatory response.7,8 Macrophages upregulate NF-κB and secrete inflammatory cytokines like IL-1β, TNFα, IL-6, and IL-8.9 Other anti-inflammatory cytokines such as IL-10 modulate the inflammatory process.
More recently, several mediators known to be involved in regulation of osteoclast differentiation and maturation, such as “Receptor Activator of NF-κB Ligand (RANKL) and osteoprotegerin (OPG, also known as osteoclastogenesis inhibitory factor (OCIF)), have been suggested as key factors in the development and progression of bone loss. Other factors involved within bone resorption include the enzymes responsible for catabolism of the organic components of bone. These include the matrix metalloproteinases collagenase (MMP-1) and stromelysin (MMP-3). All this severely affects the highly orchestrated function of osteoblasts and osteoclasts and concomitantly causing osteolysis. This PPOL at the bone-implant interface leads to an increasing instability of the implant stem within the proximal medullar cavity of the femur and/or the implant cup within the acetabulum provoking more wear for example, based on enhanced micromotions (AL) ending in a vicious cycle and finally causing progressive implant failure making a revision necessary.
Diminishing problems associated with implanted joint prosthesis
In order to generate a solution for this challenge of modern arthroplasty, a consortium of 11 research partners led by the Fraunhofer Institute for Production Technology IPT (Aachen, Germany) have now joined forces to develop a new generation of endoprostheses for the treatment of aseptic loosening disease. Within a large EU-funded Research Innovation Action (RIA) project called ‘Extracellular Vesicles Promoted Regenerative Osseointegration’ (EVPRO), the consortium aims to counteract the shortened lifetime and to reduce the risk of inflammation of hip revision prostheses.
The 11 project partners from four countries intend to ensure mobility for older patients and improve their quality of life and well-being by diminishing problems associated with implanted joint prosthesis and by reducing the number and frequency of subsequent medical treatments. The team consisting of scientists, engineers and clinicians hope that EVPRO’s results will lead to a significant decrease in aseptic loosening in joint replacement.
The objective of EVPRO is to devise new biologically active coatings for hip revision endoprosthesis able to control inflammation at the biointerface of the endoprosthesis and promote bone regeneration. The EVPRO coating combines a novel bioinstructive, adaptive nano-functionalised degradable biomaterial homing extracellular vesicles incorporated in a non-degradable bone-instructive macroporous and nano-roughened TiO2 surface. These coatings are applied exactly at the interface between the implant and inflamed bone to perceive inflammation and modulate it in a proportional, self-regulating manner.
Furthermore, the bioactive moieties instruct osteoblasts (simply expressed bone forming cells) to migrate into the coating to improve osseointegration and to achieve better healing and increased lifetime of the implant.
In the long term, the researchers expect that the number of repeated operations to replace worn implants will decrease, having a direct positive impact on the duration of the necessary hospital stay and the prescription of expensive medication. The results of the EVPRO research project can therefore support the objectives on active ageing in society and lead to significant improvements in the quality of life for hundreds of thousands of citizens in the EU and beyond.
However, it should be noted that although the EVPRO technology is still at an early stage, it has the potential to revolutionise medical technology in modern arthroplasty improving therapies for patients suffering from aseptic endoprosthesis loosening. In addition to this, other clinical areas suffering from high inflammation rates might also benefit greatly from the project results.
The development of market-ready medical products
In co-ordination with the consortium of European universities and partners in medical device and biotechnology industries, the Fraunhofer IPT will focus on building a market leading portfolio of products, required for application in the next generation of hip revision endoprosthesis and beyond. In addition to companies using the newly developed EVPRO technology directly, the partners are already working on concepts for sales and distribution along the entire value chain.
EVPRO considers process steps of the manufacturing of implants as well as preclinical studies and later end users. As soon as the EVPRO-implants are market-ready, the partners intend to evaluate the possibility of a comparatively simple transfer from EVPRO hip implant coatings to primary and secondary knee implants, which bear a market potential of more than €3.2m in the EU and the US per year. As a logical extension for a later stage utilisation analysis, further joint replacements such as shoulder, ankle or elbow replacements could also directly benefit from the EVPRO technology.
Additionally, clinical areas connected with high inflammation rates for further EV-loaded products such as intramedullary nails or dental implants, connectors such as screws or nails, and wound dressings for chronic wounds or serious burns represent a promising and broad chance for further exploitation of the EVPRO technology.
Partners in the EVPRO consortium:
Universitätsklinikum Essen
Essen, Deutschland,
(Bernd Giebel, Verena Börger, Stefan Landgräber).
Lonza Netherlands B.V.,
Maastricht, Niederlande,
(Bart van Dijk, Birgit Nelsen-Salz).
Dublin City University,
Dublin, Ireland,
(Damien King, Paul Cahill).
Trinity College Dublin,
Dublin, Ireland,
(Lorraine O´Discroll).
Leibniz-Institut für interaktive Materialien,
Aachen, Deutschland,
(Barbara Dittrich, Cesar Rodriguez-Emmenegger).
Universität Maastricht,
Maastricht, Niederlande,
(Daniel Molin, Nynke van den Akker).
Meotec GmbH & Co. KG,
Aachen, Deutschland,
(Christoph Ptock).
Stryker B.V.,
Amsterdam, Niederlande,
(Eric Garling).
Polytecnico di Torino,
Turin, Italien,
(Gianluca Ciardelli, Valeria Chiono).
Universitätsklinikum
Knappschaftskrankenhaus Bochum,
Bochum, Deutschland,
(Jochen Salber, Siegfried Shah, Richard Viebahn).
Fraunhofer Institut für Produktionstechnologie IPT Aachen
Aachen, Deutschland,
(Bastian Studerus, Claudia Skazik-Voogt).
References
- www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions
- statista.com. OECD report 2017
- https://www.eprd.de/de/
- Kurtz, S., Ong, K., and Lau. E. et al. 2007. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. Journal of Bone and Joint Surgery—Series A,vol.89,no.4,pp. 780–785
- Martinon, F., Pétrilli, V., and Mayor, A. et al. 2006. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006; 440(7081): 237-41. Epub 2006 Jan 11
- Medzhitov, R. 2008. Origin and physiological roles of inflammation. Nature. 2008; 454(7203): 428-35. doi: 10.1038/nature07201
- Mariathasan, S., Newton, K., and Monack, D.M. et al. 2004. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 2004; 430(6996): 213-8. Epub 2004 Jun 9.
- Mariathasan, S., and Monack, D.M. 2007. Inflammasome adaptors and sensors: intracellular regulators of infection and inflammation. Nat Rev Immunol. 2007; 7(1): 31-40
- Jacobs, J.J., Roebuck, K.A, and Archibeck, M. et al. 2001. Osteolysis: basic science. Clin Orthop Relat Res. 2001; (393): 71-7
Dr Jochen Salber (PhD, MD)
Senior Physician Surgery
Head of the Department of
Experimental Surgery
Department of Surgery
University Medical Centre Knappschaftskrankenhaus Bochum
Hospital of the RUHR
University Bochum
+49 234 32 21819
jochen.salber@rub.de
www.kk-bochum.de
www.researchgate.net/lab/
Jochen-Salber-Lab
Please note, this article will also appear in the first edition of our quarterly publication, the Innovation Platform.